On the week I am writing this post auto-scheduled for later publication, I am observing what so often goes on in news reporting about science: a host of science news sites mindlessly parroting the unjustified claims of a university press release. You would think that by now our science journalists might have learned the lesson that university press releases these days are often notorious for their hype, errors and misinformation, and that the claims of such press releases should be subjected to critical scrutiny.
The unfounded claim this week is one that at-home magnetic brain stimulation "shows promise" for treating depression. The claims come from a Kings College press release here, which is entitled "At home brain stimulation for depression found to be safe and effective." We have a discussion of a new study testing at-home head gadgets using something called transcranial direct current stimulation (tDCS),
The press release states this:
"Transcranial direct current stimulation (tDCS) is a form of self-administered, non-invasive brain stimulation that applies a weak, direct current of between 0.5 to 2 milliampere to the scalp via two electrodes. It is not electroconvulsive therapy (ECT), which delivers about 800 milliamperes to the brain causing a generalised seizure and can only be conducted under strict supervision.
174 participants aged 18 and over, and with a diagnosis of at least moderate depression were randomly assigned to one of two treatment arms; 'active' tDCS or 'inactive' tDCS which was the same device but did not provide a current. Participants had a 10-week course of treatment, initially having five 30-minute sessions a week for the first three weeks, followed by three 30-minute sessions a week for the following seven weeks.
Researchers found that participants in the active arm of the trial showed significant improvements in the severity of their depression, as well as the overall clinical response and remission compared to those in the ‘inactive’ placebo control arm. The rates of treatment response and remission were three times higher in the active treatment arm compared to the placebo arm, where 44.9% in the active arm demonstrated a remission rate compared to 21.8% of the control group."
A study like this attempts to follow the conventions of randomized controlled trials (RCT) using placebos. In such studies patients are randomly assigned to either a medication group or a placebo group. Typically the medication group gets some medicine being tested, and the placebo group gets only a similar-looking placebo pill that is something like a sugar pill that looks just like the real medicine. The patient does not know which group he belongs to, and does not know whether the pill he is being given is just a placebo sugar pill. Such a lack of knowledge is called an example of blinding. Such a randomized control trial attempts to see some medical outcome in the group getting the real medication that is superior to the medical outcome reported in the placebo group. When both a doctor or scientist and the patient are unaware (for at least part of the time) whether particular patients belong to the get-the-real-treatment group or the placebo control group, such a study is called a "double-blind" study.
The press release quoted above refers to the study here, entitled "Home-based transcranial direct current stimulation treatment for major depressive disorder: a fully remote phase 2 randomized sham-controlled trial." The study claims to have been a double-blind study, saying that it was a "fully remote, multisite, double-blind, placebo-controlled, randomized superiority trial." But the claim about being double-blind is not correct. The patients who were supposed to be blind as to whether or not they were getting the real magnetic stimulation were not really blind about such a thing.
The failure of the blinding protocol to achieve real blindness (a lack of knowledge by subjects about whether they were receiving the real treatment) is shown by the section of the paper entitled "Analysis of study blinding and unblinding." There we read this:
"Before unblinding at week 10 (end of trial), participants were asked to guess whether they thought they were receiving the active or sham tDCS device and their level of certainty, rating from ‘1’ for ‘very uncertain’ to ‘5’ for to ‘very certain’. A guess of active tDCS was made by 77.6% in the active treatment arm and 59.3% in the sham treatment arm; the difference was significant (P = 0.01)."
This is a very big difference. 77% of the people getting the real treatment thought they were getting the real treatment, but only 59% of the people in the "no treatment" placebo group thought they were getting the real treatment. This indicates a very major effect in which the people getting the real treatment were much more likely to think that they were getting the real treatment than those not getting the real treatment. In a randomized control trial that achieves an effective level of blinding, there will be no difference between the percentage of real-treatment subjects and placebo or sham treatment subjects who thought they were getting the real treatment.
Analyzing the paper, it's easy to see why patients who were not getting the real treatment would have been been better able to figure out whether they were getting the real treatment. We read this:
"Active stimulation consisted of 2 mA direct current stimulation for 30 min with gradual ramp up over 120 s at the start and ramp down over 15 s at end of the session. Sham stimulation with the same device and app was used to resemble the active intervention and to receive the treatment schedule. An initial ramp up from 0 to 1 mA over 30 s then ramp down to 0 mA over 15 s was repeated at the end of the session to cause a tingling sensation that mimics active stimulation."
So the people getting the real treatment got 30 minutes of real direct current stimulation of their head, but the people getting the sham or placebo treatment got only about 30 seconds of real direct current stimulation. Such a big difference helps explains why a much higher percentage of those getting the real treatment thought they were getting the real treatment.
That much higher percentage is enough to explain the difference in the reported relief of depression symptoms, even while assuming that the head device had zero real effectiveness in treating depression. Being much more likely to think that they had got some possibly effective real brain zapping effect, the people in the real treatment group were much more likely to get a placebo effect that was largely the power of suggestion. Similarly, assign two groups of patients sugar-pill placebos, telling the first group that the pill is a powerful anti-depressant, and the second that the pill is just a vitamin, then the first group will probably report significant improvement in their depression, because of placebo effects and the power of suggestion.
Nowadays biotech companies may have a very large incentive to fund and/or promote poorly designed and executed brain research, particularly whenever such research helps to promote some device that such companies sell. Biotech companies include very many companies such as the manufacturers of MRI devices, the manufacturers of EEG equipment, the manufacturers of implantable medical devices, and the manufacturers of noninvasive brain-related devices that a person may put on his head. The biotech industry is a trillion-dollar industry, and many billions of that involves brain-related products.
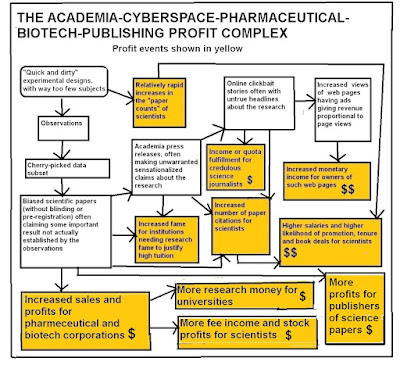
Neuroscientists these days are thoroughly entangled with pharmaceutical companies and the manufacturers of biotech devices. The entanglement casts great doubt on the objectivity of any such scientists doing studies relating to the effectiveness of any brain-related medicine or any brain-related medical device. These entanglements and their pernicious effects on the objectivity of neuroscientists is discussed in my post "How the Academia-Cyberspace-Pharmaceutical-Biotech-Publishing Complex Incentivizes Bad Brain Research," which you can read
here.
The diagram below illustrates some of the entanglements and conflicts of interest going on:
Whenever you read a science paper that seems to promote some medicine or medical device, it is always a good idea to study the "Competing Interests" section of the paper, in which scientists are supposed to reveal possible conflicts of interest that may have affected their objectivity. When you examine that "Competing Interests" section of the paper being discussed, all kinds of alarm bells should go off. Here it is:
"C.H.Y.F. reports the following competing interests: research grant funding on behalf of the University of East London from Flow Neuroscience (no. R102696); research grant funding from NIMH (no. R01MH134236), the Baszucki Brain Research Fund Milken Institute (no. BD0000009), the Rosetrees Trust (no. CF20212104), the International Psychoanalytic Society (no. 158102845), the MRC (no. G0802594), NARSAD and the Wellcome Trust. She is Associate Editor of Psychoradiology and Section Editor of the Brain Research Bulletin. A.H.Y. reports the following competing interests: paid lectures and advisory boards for the following companies with therapies used in affective and related disorders: Flow Neuroscience, Novartis, Roche, Janssen, Takeda, Noema Pharma, Compass, AstraZeneca, Boehringer Ingelheim, Eli Lilly, LivaNova, Lundbeck, Sunovion, Servier, LivaNova, Janssen, Allegan, Bionomics, Sumitomo Dainippon Pharma, Sage, Novartis and Neurocentrx. He is principal investigator for the following studies: the Restore-Life VNS registry study funded by LivaNova; ESKETINTRD3004: ‘An Open-label, Long-term, Safety and Efficacy Study of Intranasal Esketamine in Treatment-resistant Depression’; The Effects of Psilocybin on Cognitive Function in Healthy Participants; The Safety and Efficacy of Psilocybin in Participants with Treatment-Resistant Depression (P-TRD); A Double-Blind, Randomized, Parallel-Group Study with Quetiapine Extended Release as Comparator to Evaluate the Efficacy and Safety of Seltorexant 20 mg as Adjunctive Therapy to Antidepressants in Adult and Elderly Patients with Major Depressive Disorder with Insomnia Symptoms Who Have Responded Inadequately to Antidepressant Therapy (Janssen); An Open-label, Long-term, Safety and Efficacy Study of Aticaprant as Adjunctive Therapy in Adult and Elderly Participants with Major Depressive Disorder (MDD) (Janssen); A Randomized, Double-blind, Multicentre, Parallel-group, Placebo-controlled Study to Evaluate the Efficacy, Safety, and Tolerability of Aticaprant 10 mg as Adjunctive Therapy in Adult Participants with Major Depressive Disorder (MDD) with Moderate-to-severe Anhedonia and Inadequate Response to Current Antidepressant Therapy; A Study of Disease Characteristics and Real-life Standard of Care Effectiveness in Patients with Major Depressive Disorder (MDD) With Anhedonia and Inadequate Response to Current Antidepressant Therapy Including an SSRI or SNR (Janssen). He is UK Chief Investigator for the following studies: Novartis MDD study no. MIJ821A12201; Compass; and the COMP006 and COMP007 studies. Grant funding (past and present) includes: NIMH (USA); CIHR (Canada); NARSAD (USA); the Stanley Medical Research Institute (USA); MRC (UK); the Wellcome Trust (UK); the Royal College of Physicians of Edinburgh; the British Medical Association (UK); the VGH & UBC Foundation (Canada); WEDC (Canada); the CCS Depression Research Fund (Canada); the Michael Smith Foundation for Health Research (Canada); NIHR (UK). Janssen (UK) and EU Horizon 2020. He is the Editor of the Journal of Psychopharmacology and Deputy Editor of BJPsych Open. He has no shareholdings in pharmaceutical companies. S.S. reports the following competing interests: research grant funding on behalf of the University of Texas Health Science Center at Houston from Flow Neuroscience; paid advisory boards for the following companies: Worldwide Clinical Trials and Inversago; and Vicore Pharma. He is a full-time employee of Intra-Cellular Therapies. He has received grants and research support from NIMH (USA) (no. 1R21MH119441-01A1), NIMH (no. 1R21MH129888-01A1), NICHD (no. 1R21HD106779-01A1), SAMHSA (no. 6H79FG000470-01M003) and Fizer foundation. He has received research funding as a principal investigator or study/subinvestigator from or participated as consultant/speaker for Flow Neuroscience, COMPASS Pathways, LivaNova, Janssen, Relmada and the Psychiatry Education Forum. Intra-Cellular Therapies or National Institutes of Health (NIH) or SAMHSA or any other organizations had no role in study design and conduct; the collection, management, analysis and interpretation of the data; the preparation, review or approval of the manuscript; and the decision to submit the manuscript for publication. The study’s content is solely the responsibility of the authors and does not necessarily represent the official views of the Intra-Cellular Therapies or NIH or SAMHSA. R.M-V. has received consulting fees from Eurofarma Pharmaceuticals, Abbott and BioStrategies group; has research contracts with Boerhinger Ingelheim and Janssen Pharmaceuticals; and has received speaker fees from Otsuka, EMS and Cristalia. He is a member of the scientific boards of Symbinas Pharmaceuticals and Allergan. He is also the principal investigator for the following grants: NIH (nos. R21HD106779 and R21MH129888), Milken Institute (no. BD-0000000081). D.M. and L.H. work for Biomedical Statistical Consulting; they provide statistical support to MCRA and received payments from Flow Neuroscience. A.-R.G.-N., G.S., H.H., J.C.S., M.R., N.L., P.J.L., P.O., R.D.W. and S.S.K. declare no competing interests."
What is this Flow Neuroscience we keep hearing about? It is a manufacturer of a head-zapping device marketed as an aid for depression -- exactly the type of device being promoted by this poorly designed and unconvincing study. We should not expect scientists taking lots of money from some manufacturer to produce unbiased studies evaluating a device of such a manufacturer.
Under the assumptions of materialism, the idea that you could improve your health by zapping your brain with electricity or magnetism makes no sense. Under the assumptions of materialists, we might expect that zapping your brain might disrupt the "delicate brain mechanism of memory storage" that materialists believe in. Luckily such devices probably don't harm your memories, because such memories are not actually stored in your brain. It is ironic for neuroscientists to be promoting devices doing brain-zapping that make no sense under the assumptions of such neuroscientists. Maybe when they promote such devices, somehow they are recalling the utter failure of neuroscientists to present a credible theory of brain memory storage or brain instant recall, and the utter failure of neuroscientists to find any trace of learned human knowledge by microscopic examination of brain tissue.
They are "in bed with each other"
Postscript: A slightly different method uses alternate current rather than direct current, and is called Transcranial Alternate Current Stimulation or tACS. A year 2025 review paper states, " Overall, tACS has minimal impact on working memory improvement, but it shows potential under certain conditions. "

No comments:
Post a Comment