I was previously asked by some of my readers for comments on the paper "A Neuroscientific Model of Near-Death Experiences." At that time I did not critique the paper because it was behind a paywall, and the abstract gave no reason for suspecting that the paper was worth a 20 dollar payment. The paper is now publicly available at the link here (alternate link here). We have a paper that claims to have a "model" of near-death experiences, but actually offers no physically realistic model of any such thing. What we get is a jargon-filled jumble that does nothing to explain any of the main features of near-death experiences. The abstract gives a clue of the hodgepodge farrago that the paper is, by saying that it will offer "a model for NDEs that encompasses a cascade of concomitant psychological and neurophysiological processes within an evolutionary framework." So the strategy is apparently something like: let's sprinkle some psychology talk with some brain chemistry talk and some Darwinist evolutionary biology talk, and see whether that adds up to an explanation for near-death experiences. The result resembles someone wildly firing shots in all different directions.
The co-authors start out by giving us a three-paragraph discussion entitled "Cerebral blood flow, blood gases and neuronal function." Here is the first paragraph:
"Just before and during cardiopulmonary arrest, cerebral blood flow is compromised, resulting in a swift decline in oxygen and glucose supplies and an accumulation of CO2. Oxygen deprivation (hypoxia) impairs cellular respiration and ATP production, thereby disrupting energy-dependent cellular processes. This deprivation also affects the function of enzymes such as monoamine oxidase (MAO), which is responsible for degrading monoamine neurotransmitters, including serotonin, dopamine, noradrenaline and histamine. In addition, elevated CO2 levels (hypercapnia) contribute to acid–base imbalance. CO2 combines with water to form carbonic acid (H2CO3), which dissociates into H+ and HCO3 – ions. During hypercapnia, the buffering capacity of HCO3 – is exceeded by an overabundance of H+ , leading to decreased pH43, disrupted ATP production, and cerebral acidosis. Reductions in brain pH activate acid-sensing ion channels (ASICs), leading to an influx of Na+ ions, which further contributes to neuronal depolarization and the triggering of action potentials."
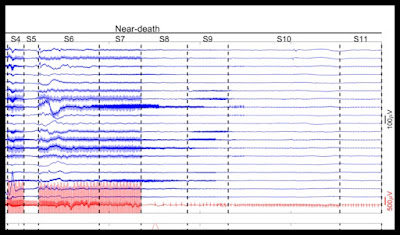
We have lots of mention of chemistry details, a jargon-filled discussion that is meant to impress us. But it should not impress us in the least, because it has no relevance to explaining near-death experiences. There is one main relevant neuroscience-related fact here (which the paper fails to ever mention). It is that very soon after the heart stops beating during cardiac arrest, the brain shuts down electrically. This is shown in EEG readings, which show the brain flatlining within 10 to 20 seconds after cardiac arrest. When this flatlining of brain signals occurs, the normal wavy appearance of brain waves become flat lines.
The term "isoelectric" or iso-electric in reference to brain waves means a flat-lining equivalent to no electrical activity in the brain, as measured by EEG readings. The paper here states, "Within 10 to 40 seconds after circulatory arrest the EEG becomes iso-electric." Figure 1 of the paper here says that such an isoelectric flat-lining occurred within 26 seconds after the start of ventricular fibrillation, the "V-fib" that is a common cause of sudden cardiac death, with "cortical activity absent." Also referring to a flat-lining of brain waves meaning a stopping of brain electrical activity, another scientific paper says, "several studies have shown that EEG becomes isoelectric within 15 s [seconds] after ischemia [heart stopping] without a significant decrease in ATP level (Naritomi et al., 1988; Alger et al., 1989)." Another paper tells us this about brain waves and infarction (obstruction of blood flow), using CBF to mean cerebral blood flow, and the phrase "the EEG becomes isoelectric" to mean a flat-lining of brain electrical signals:
"When normal CBF declines, the EEG first loses the higher frequencies (alpha and beta bands), while the lower frequencies (delta and theta bands) gradually increase. When the CBF decreases further towards an infarction threshold, the EEG becomes isoelectric."
Similarly, another paper refers to blood pressure, and tells us, "When flow is below 20 mL/100 g/min (60% below normal), EEG becomes isoelectric." meaning that brain electrical activity flat-lines. The 85-page "Cerebral Protection" document here states, "During cardiac arrest, the EEG becomes isoelectric within 20-30 sec and this persists for several minutes after resuscitation." Another scientific paper states this:
"Of importance, during cardiac arrest, chest compliance is not confounded by muscle activity. The EEG becomes isoelectric within 15 to 20 seconds, and the patient becomes flaccid (Clark, 1992; Bang, 2003)."
The fact of the brain flatlining and becoming isoelectric within about 10 to 20 seconds of cardiac arrest is an all-important fact in any neuroscience attempt to explain near-death experiences. It means that all such attempts are doomed to failure. There can be no brain explanation of some mental phenomenon if that phenomenon occurs when the brain is electrically inactive. Similarly, you can have no explanation of your computer performing some task if the task occurred while your computer was unplugged and your computer has no batteries.
Does the paper "A Neuroscientific Model of Near-Death Experiences" ever tell us this all-important fact that brains become isoelectric (electrically inactive) within a few seconds after cardiac arrest? No, it does not. The paper does not use the word "isoelectric" and does not use the word "flatline." The paper makes no reference to EEG readings, and no reference to brain waves. The text of the paper fails to use the term "EEG" and fails to use the term "brain wave." So the paper's pretensions to be describing what goes on in a brain during cardiac arrest is a sham. The authors have ignored the most fundamental reality of what goes on in a brain during cardiac arrest.
The vast majority of the paper "A Neuroscientific Model of Near-Death Experiences" is a discussion of brain chemicals. Before reviewing this discussion I can give some background information on that topic. The main chemicals the paper discusses are serotonin, glutamate, noradrenaline, acetylcholine, endorphins, dopamine and GABA. These chemicals are found in extremely tiny amounts such as 1 part per million in brain fluid. Prior to the past few years, there did not exist any reliable method for accurately measuring increases in such chemicals occurring over a very short time span such as the few minutes following the beginning of cardiac arrest. There existed a technique called microdialysis, which involved inserting a needle or tube into the brain, and taking fluid from some tiny part of it. Such a technique was not suitable for reliably tracking changes in brain chemicals over a short period. Someone might try to insert such microdialysis needles three times in quick succession over a period such as ten minutes, and then analyze the extracted fluid. But any differences reported would be more likely to be due to region-to-region variations in such chemicals, or uncertainties in the attempted measurements themselves, rather than an actual increase over the short time span. The identification of chemicals existing in only extremely tiny trace amounts is an affair involving large chances for error, with uncertainties often spanning several orders of magnitude, between 10 and 1000 times. For example, the paper here lists studies that attempted to measure one brain chemical by using microdialysis, and the reported results vary between 1 nanomole and 2000 nanomoles.
Whenever we hear any claims that some brain chemical was found to increase during ischemia (the blockage of blood to the brain), we should always ask questions such as these:
(1) How many studies reported such an effect, and were the study group sizes used sufficient to produce a high statistical power?
(2) What fraction of the brain was checked? Was it only a hundredth of the brain, such as only the striatum or the hippocampus?
(3) What was the time scale? Was it over hours or days (irrelevant for discussions of near-death experiences), or was it over some very short time scale that might be relevant to explaining something going during cardiac arrest or near-death experiences?
Almost always the answers to these questions will deflate any claims to have found a relevant surge in brain chemicals, showing that the claims are not well founded and not well replicated.
Here are some of the sections in the paper "A Neuroscientific Model of Near-Death Experiences":
- The section entitled "the serotonergic system." We have eight paragraphs describing the role of serotonin in the brain. None of the discussion has any relevance to explaining any of the more interesting features of near-death experiences. Serotonin does not produce hallucinations. The paper "Serotonin and Human Cognitive Performance" discusses the results of "experimental studies involving healthy human volunteers," but makes no mention of hallucinations in these volunteers who had their serotonin levels artificially increased. Millions of people in the US take SSRI drugs that are specifically designed to increase serotonin levels; but such drugs do not produce hallucinations. The paper here (discussed in the appendix) involved experiments that increased by very many times (between 100 times and 1000 times, in other words 10000% to 100000%) the serotonin levels in volunteers, by infusions of serotonin. No hallucinations were reported. There is no robust evidence that serotonin surges in humans during near-death experiences or during cardiac arrest. The paper "A Neuroscientific Model of Near-Death Experiences" makes the claim that "In rats undergoing asphyxia, a dramatic initial surge in brain serotonin levels was observed — up to 100–200 times higher than baseline." This is a reference to a 2015 paper that did not reliably observe any such thing, because at the time there was no reliable technology for measuring short-term spikes in serotonin levels, and the study group size was way too small (only 7 rats) for a reliable result to be claimed. The paper used a microdialysis and liquid chromatography-mass spectrometry (LC-MS) method that at the time was not very reliable because of reasons discussed in the appendix of this post. After giving us detail after detail about serotonin, none of which have any relevance to explaining near-death experiences, the section drifts off to a discussion of other topics such as DMT trips and speculations about evolution. The section has no relevance to explaining near-death experiences. A 2025 paper highlighting the unreliability of serotonin measurements is entitled "The Continued Mismeasurement of Plasma Serotonin: A Systematic Review." It states this: " The review covered the period from 2010 to July 2024 and is a follow-up of a similar review published in 2011 which found that nearly all published reports of PPP 5-HT [serotonin] were clearly and markedly erroneously high. This problem has persisted unabated with nearly all retrieved 47 reports from the past 14 years also apparently being erroneously high."
- The section entitled "the glutamatergic system." We have five paragraphs discussing the role of the neurotransmitter glutamate in the brain. None of it has any relevance to explaining near-death experiences. Senselessly the authors try to use this discussion as a launchpad for discussing ketamine, a hallucinogenic drug. This goes nowhere, because the authors confess that while someone "hypothesized that in life-threatening situations, an endogenous ketamine-like neurotoxin might be released," the fact is that "no empirical evidence has been found to support the existence of such a molecule." The authors attempt to insinuate that during cardiac arrest there may be a big increase in glutamate. There is no robust evidence that this is true, and if it were true, it would be irrelevant, because glutamate is not any type of hallucinogen. As I discuss in my post "The Groundless Myth That 'Floods'' or 'Surges' Help Explain Near-Death Experiences," there is no evidence that any type of relevant brain chemical surges during cardiac arrest or near-death experiences. Claims of such a surge is a deceptive element repeated again and again in articles or papers attempting to explain near-death experiences. There are two very strong reasons why such claims must be wrong or irrelevant. The first fact is that we know that neurotransmitters are synthesized at a very slow rate, making unbelievable all claims of a sudden surge in neurotransmitters at death. The second fact (supremely relevant but senselessly ignored by the co-authors of the paper "A Neuroscientific Model of Near-Death Experiences") is that brains become isoelectric (i.e. they flat-line) within 10 to 20 seconds of cardiac arrest, making all claims about neurotransmitter increases at such a time irrelevant or unbelievable.
- The section entitled "the noradrenergic system." We have three paragraphs giving an irrelevant discussion of a chemical called noradrenaline. The attempt to link this discussion to near-death experiences is feeble and laughable. We have the claim that "noradrenaline might also aid memory consolidation though its effect on the amygdala" and that "the ability of humans to recall vivid memories even on the verge of death could be explained by high noradrenaline levels during asphyxia." The statements are nonsensical. There is no evidence that memory recall is increased when people have higher levels of noradrenaline. The relevant fact here (completely ignored by the authors) is that during cardiac arrest brain waves very quickly become isoelectric, and that brains shut down electrically and flatline, something that (under assumptions brains store memories) should completely prevent the formation of any new memories. Instead of there being a neuroscience reason why someone might form vivid memories during cardiac arrest, there is the strongest neuroscience reason why such a thing should be impossible under the assumptions of neuroscientists.
- The section entitled "the cholinergic system." We have two paragraphs discussing the neurotransmitter acetylcholine. We have the unfounded claim that acetylcholine enhances memory formation. Neuroscientists do not have any credible theory of memory formation, and there is no strong evidence that increased acetylcholine levels cause higher levels of memory formation. The attempt in the paper to link acetylcholine to near-death experiences is a feeble one: merely something like insinuating that acetylcholine helps memory, and that acetylcholine might help someone remember a near-death experience. The authors continue to be utterly oblivious to the most relevant fact here: that when a brain is isoelectric, in an EEG-flatline state and not generating any brain waves, the formation of memories should be impossible under "brains store memories" assumptions.
- The section entitled "the endorphinergic system." We have three paragraphs discussing endorphins, a type of brain chemical widely discussed as a "feel good" kind of chemical. We have the incorrect claim that a study showed that endorphins increase in dogs undergoing sudden cardiac death. The reference is to a 1995 paper that should never be cited as credible evidence for such a claim. In 1995 there did not exist any reliable technology for measuring very short-term spikes in brain chemicals in animals such as dogs. The paper does not mention any study group size, and we may assume that it was one of innumerable neuroscience experiments using a study group size way-too-small for a reliable result to be claimed. Here we must remember that if people had reliable evidence for the claim that endorphins increase during sudden cardiac death, they would be citing papers of recent decades, not papers from 30 years ago. The attempt to link endorphins to near-death experiences is a feeble one: merely the suggestion that endorphins might help explain mood elevation.
- The section entitled "the dopaminergic system." The brain chemical discussed is dopamine. We again have a dubious claim that such a chemical was found to have increased in dying rats. The claim is based on the 2015 paper here, the paper "Asphyxia-activated corticocardiac signaling accelerates onset of cardiac arrest." At that time there did not exist any reliable methods for making real-time in vivo measurements of brain chemicals over short periods of time such as ten minutes. The technique used by the paper (microdialysis and liquid chromatography-mass spectrometry or LC-MS) was not suitable for accurately measuring real-time changes in neurotransmitters over a tiny time scale such as 10 minutes. (See the appendix for more on the problems with LC-MS.) The paper cited was not a robust science paper because of its use of way-too-small study group sizes such as only 7 rodents. One of the co-authors of the "A Neuroscientific Model of Near-Death Experiences" paper (Martial) makes a misstatement about a previous paper of hers, claiming, "Martial et al. found that coma survivors who reported NDEs exhibited suboptimal source monitoring and an increased tendency to illusory recollection, compared with those without NDEs." To the contrary, the paper in question (doing some memory test on 20 subjects reporting a near-death experience and 20 who did not) reported "we obtained equivalent proportions of correct and false recall performance in both groups." The section attempts to insinuate that dopamine causes hallucinations. There is no strong evidence that dopamine causes visual hallucinations. The paper "Effects of Dopamine in Man" reports on the effects of 13 subjects who were given a 1% infusion of dopamine, causing dopamine levels many times higher than naturally occur. The paper makes no mention of any hallucinatory effects or any mental effects. A similar experimental result (reporting no hallucinations) is reported in the paper here, which tested artificially produced dopamine spikes as high as 1000 times higher than normal. Attempts to claim dopamine levels have an association with the merely auditory hallucinations of schizophrenia are advanced by pharmaceutical companies and neuroscientists financially entangled with them, who are interested in selling pills that supposedly affect dopamine levels. The claim is irrelevant, because of the lack of robust evidence that dopamine sharply increases in humans during sudden cardiac arrest or near-death experiences (outside of perhaps one or two small areas in the middle of the brain like the striatum), the implausibility of the claim that it could very quickly increase during such rapid events (given the very slow production rate of all neurotransmitters), the fact that brains that quickly flatline a few seconds after cardiac arrest cannot be hallucinating brains, and the fact that very strong dopamine infusions in humans do not produce hallucinations. No one has ever caused someone to have a visual hallucination by giving him an injection or infusion of dopamine.
- The section entitled "the gabaergic system." We have two paragraphs discussing GABA, neither of which discuss any convincing link between such a chemical and near-death experiences.
- "I sometimes feel that I have had an out-of-body experience."
- "During my life I have had intense religious experiences which influenced me in a very strong manner."
- "I often have the experience of thinking of someone and soon afterwards that person calls or shows up."
- There is no robust evidence that serotonin very sharply increases in the human brain during cardiac arrest or near-death experiences, and if it were to increase, that would do nothing to explain near-death experiences, because serotonin is not a hallucinogen, and brains are electrically shut down during cardiac arrest. The paper here (discussed in the appendix) involved experiments that increased by very many times (between 100 times and 1000 times, in other words 10000% to 100000%) the serotonin levels in volunteers, by infusions of serotonin. No hallucinations were reported.
- There is no robust evidence that glutamate increases in the brain during cardiac arrest or near-death experiences, and if it were to increase, that would do nothing to explain near-death experiences, because glutamate is not a hallucinogen, and brains are electrically shut down during cardiac arrest. One paper says, "Many preclinical studies revealed decreased glutamate whole tissue content after ischemia."
- Because adrenaline is often injected into people undergoing cardiac arrest to try and stop such an arrest, there may be noradrenaline increases in the brain during some cardiac arrest cases and near-death experiences. But that does nothing to explain near-death experiences, because noradrenaline is not a hallucinogen, and brains are electrically shut down during cardiac arrest.
- There is no good evidence that acetylcholine increases in the brain during cardiac arrest and near-death experiences, and if it were to increase, that would do nothing to explain near-death experiences, because acetylcholine is not a hallucinogen, and brains are electrically shut down during cardiac arrest.
- There is no strong evidence that endorphins increases in the brain during cardiac arrest and near-death experiences, and if endorphins were to increase during such events, that would do nothing to explain near-death experiences, because endorphins are not a hallucinogen.
- Discounting some not-very-convincing studies (with too-small study group sizes) that may suggest an increase in dopamine in two tiny regions of the brain (the striatum and the hippocampus) of rats during ischemia, there is no robust evidence that dopamine very sharply increases in the human brain during cardiac arrest and near-death experiences; and if it were to increase, that would do nothing to explain near-death experiences, because while hypothesized (without strong evidence) to be more common in some who have auditory hallucinations, dopamine is not a cause of suddenly appearing visual hallucinations, because very strong infusions of dopamine in humans do not produce any hallucinations or mental effects, and because brains are electrically shut down during cardiac arrest.
- There is no robust evidence that GABA increases in the brain during cardiac arrest and near-death experiences, and if it were to increase, that would do nothing to explain near-death experiences, because GABA is not a hallucinogen, and because brains are electrically shut down during cardiac arrest.
"However, application of this technology is not automatically or necessarily translated into accurate results. Its pitfalls have to be recognized and must be addressed systematically. In particular interferences from in-source transformation of metabolites, differential matrix effects of analyte and internal standard and isobaric transitions can lead to inaccurate results of LC-MS/MS analyses."
A similar paper discusses at great length many pitfalls and ways-to-go-wrong using this method, stating "We observed cases of false-positive results with the use of liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS)." Still another paper (on page 109 of the document here) refers to an "Achilles heel" of this liquid chromatography-mass spectrometry method (LC-MS), saying the problem can lead to "gross errors" when trying to measure the levels of some chemical in a sample. The same document tells us on page 120 that "it must be emphasized that the risk of gross errors is probably higher for LC-MS/MS compared to analyses run on standard clinical chemistry analyzers."
Mass spectrometry does not measure the levels of neurotransmitters in a sample. As a wikipedia.org article tells us, "Mass spectrometry (MS) is an analytical technique that measures the mass-to-charge ratio (m/z) of charged particles (ions)." Attempting to deduce changes in very tiny levels of a particular neurotransmitter chemical (over a time span of a few minutes) from mass spectrometry readings would involve guesswork and some complex and largely arbitrary analysis pathway that would be very hard to get right. To get reliable results, you would need at least three things:
(1) A sufficient sample size, such as 20 animals per study group, rather than the mere 7 animals used in the paper "Asphyxia-activated corticocardiac signaling accelerates onset of cardiac arrest."
(2) A blinding protocol which would make sure that each person analyzing extracted brain fluid had no idea where in a time sequence the sample corresponded to, to avoid some effect in which analyst bias helped produced higher estimations in later samples, to fit in with some desired "increase of neurotransmitters" narrative.
(3) An adequate replication of the results by other well-designed studies using adequate sample sizes.
Nothing of the sort occurred here. The sample size used was too small for any decent statistical power: only 7 animals. No mention is made of a blinding protocol. And the study was never replicated by additional well-designed studies.
The paper here describes experiments in which human subjects were infused with serotonin. The serotonin levels of the patients were increased by very many times. When I do a Google search for "Amount of serotonin in the blood moles per liter," I get an answer saying, "the normal range of serotonin in the blood, expressed in moles per liter, is approximately 0.00000028 to 0.00000114 mol/L" (moles per liter). The paper says that it increased serotonin levels to between .0000001 and .0001 moles per liter for 22 subjects, and that two of the subjects had their serotonin levels increased to .001 moles per liter. This was an experiment that was increasing serotonin levels in humans by a factor of between 100 times and 1000 times. No hallucinations were reported. Clearly speculations that serotonin increases during cardiac arrest might cause hallucinations are as groundless as claims that dopamine increases during cardiac arrest might cause hallucinations.
The paper here ("HUMAN BEHAVIOURAL AROUSAL INDUCED BY DOPAMINE") discusses experiments in which human subjects received dopamine infusions that increased their dopamine levels to as high as 1000 nanomoles per milliliter, which is a level more than 1000 times higher than normal. The paper fails to mention any hallucinations resulting. This is more evidence that it is senseless to try to speculate that dopamine spikes during cardiac arrest might explain near-death experiences.
One of the worst parts of the "A Neuroscientific Model of Near-Death Experiences" paper comes in a diagram in which there is a box marked "Evolutionary advantages," and we have a reference to "enabling the individual to cope with life-threatening or painful situations." Near-death experiences do nothing to increase the likelihood of surviving a life-threatening situation. Of course, someone undergoing cardiac arrest will not be more likely to survive if he has some mental experience of leaving his body while his heart has stopped. And if someone is drowning or freezing to death, it will not at all increase his chance of surviving if his life flashes before his eyes, or if he sees himself floating out of his body and encountering a mystical realm or a numinous mysterious light. Far from increasing survival rates during such events, a near-death experience would be a distraction that would lessen the chance that someone would focus on what he needs to do to save himself in such a situation. So all attempts to postulate some Darwinian "survival of the fittest" explanation for near-death experiences are nonsensical.
Postscript: Some of my complaints were similar to those in a letter published in Nature Reviews Neurology a few days before my post was published, a letter entitled "Limitations of neurocentric models for near-death experiences." The letter is behind a paywall, but without paying I can at least read that it says this about Martial's NEPTUNE "model" of near-death experiences:
"Their model, though ambitious, omits key phenomenological features that are central to the core NDE experience [near-death experiences] and overextends certain neurochemical correlates into causal explanations. In establishing their neurocentric model, Martial et al. attempt to reframe many defining features of NDEs. NDEs characteristically involve a distinct constellation of features that sets them apart from dreams, fantasies, hallucinations or epileptic phenomena. These features include veridical out-of-body observations (often corroborated by medical personnel); transitions to ‘otherworldly realms’; panoramic life reviews (including re-experiencing past events from multiple vantage points); and encounters with deceased (but not living) relatives or ‘beings of light’. Many experiencers also undergo lifelong transformative changes in personal values and a marked loss of fear of death. Such features appear with remarkable consistency across cultures and times, and merely equating them with phenomena on the spectra of hallucinations or stress-induced fantasies misses precisely what distinguishes NDEs in terms of their specificity, coherence and intensity."
After the publication of this post on 7/15/2025 there was published (in October 2025) the paper "A Neuroscientific Model of Near-Death Experiences Reconsidered" by Bruce Greyson and Marieta Pehlivanova, which is a criticism of the Martial paper criticized in my post above. You can read the paper here. The Greyson and Pehlivanova paper mostly consists of criticisms different from those I made, which is an indication of how many are the criticisms that can be made of the Martial paper and its "NEPTUNE" model. The article here summarizes the paper.

Amazing post! Thank you!
ReplyDelete